Shared on 27-02-2020
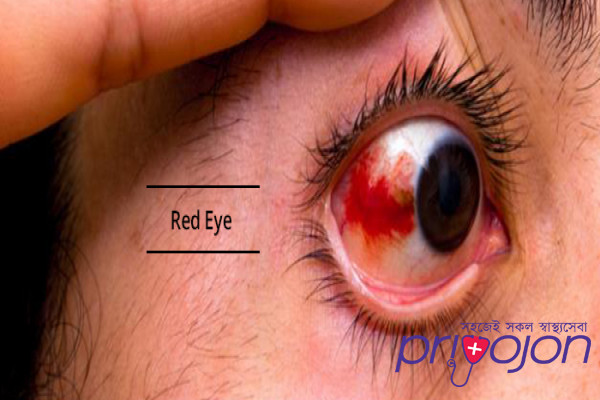
Common Causes Of Red Eye
Common Causes Of Red Eye
Throughout the year children often have eye infections, allergies, and dry eyes. Eye infections can affect one or both eyes and are most common in children. Some eye infections are highly contagious, and you must take care not to infect other people, or even your other eye if only one eye is infected. As a parent, these conditions can be alarming and it is important to know when to come see your Optometrist for evaluation. Medically necessary visits with your Optometrist for these conditions are covered by Alberta Health Care for all age groups including children.
Conjunctivitis – bacterial, allergic or viral – involves inflammation of the transparent membrane that covers the sclera and lines the eyelids.
Bacterial Conjunctiviits or “pink eye” is one of the most common and contagious eye infection particularly among school aged children. When the conjunctiva is infected, the blood vessels become irritated and swell giving the eye a red or pink appearance. Symptoms include: redness, tearing, discharge or pus (matting of the eyes with a green or yellow discharge), itching, burning sensation and light sensitivity. Antibiotics are required to eliminate the bacteria and can take up to two weeks to heal depending on the severity of the infection.
Viral Conjunctivitis is highly contagious as airborne viruses can be spread through sneezing and coughing. This condition can be seen with common viral upper respiratory infections such as the flu or the common cold causing a runny nose, cough, and/or an enlarged lymph gland in front of the ear. Symptoms include: a watery discharge, redness, blurred vision, pain, irritation and light sensitivity. The infection starts in one eye and quickly spreads to the other eye. Unlike a bacterial infection, antibiotics are not effective in treating viruses but rather the use of supportive therapies such as eye drops can help symptoms. The condition is self-limited and will go away on its own.
Allergic conjunctivitis is the result of your child’s immune system reacting to a foreign substance such as pollen, pet dander, dust, or various chemicals. Your child’s body releases histamine as part of an inflammatory response to the foreign substance causing the blood vessels in your child’s eyes to swell and become red and watery. The eyes are typically itchy with a stringy white discharge. Treatment can include having your child avoid the allergen, use of cold compresses, and/or take an antihistamine eye drop especially during allergy season. It is important to note allergic conjunctivitis can be seasonal or perennial (year-round).
Dry eyes is the result of either an insufficient quantity or quality of tears to properly lubricate and nourish your child’s eyes. Dry eyes is chronic, progressive and commonly seen in all age groups in Calgary. Risk factors include medications, contact lens use, computer use, environment, and climate. Symptoms include: blurred vision, burning sensation, dryness, grittiness, itching, sensitivity to light, redness, stinging, tired eyes, eye rubbing, soreness, and tearing. Treatment options are customizable to each child and can include the use of lubricating drops, vitamins, increasing water intake, increasing the number of breaks on the computer, using a humidifier and more.
Blepharitis is an inflammation of the eyelids resulting in redness, crusting and scaling. The eyelids may be itchy or irritated. Blepharitis is commonly seen in conjunction with dry eyes. Treatment includes daily cleansing of your child’s eyelids with lid wipes. In certain cases, an antibiotic cream may be needed. If left untreated, blepharitis can lead to the formation of a stye or chalazion.
Stye or hordeolum is caused by a bacterial infection and produces a tender, red, swollen bump on or within your child’s eyelid that is painful. A Chalazion is nodule or swollen area caused by an oil gland in the eyelid that becomes blocked. The nodule is not red and nor is it tender to touch. Both require warm compresses and sometimes topical antibiotics. In some cases, excision may be required.
Corneal Abrasion occurs after having a foreign body in the eye or scratching the eye. Symptoms include redness, pain, tearing, and sensitivity to light within your child’s eye. An abrasion can be detected by your Optometrist using fluorescein dye drops in the eye and looking at it with a special blue light. Treatment includes an antibiotic until healed.
Dacryostenosis is a blocked tear duct and is very common in newborns and infants. In most cases, the ducts open up on their own by one year of age. Signs include matting of the eye and persistent tearing in one or both eyes of your child. Parents are encouraged to wipe away (using separate cloths for each eye) any discharge with a warm cloth. Gentle massage to ducts is advised to help open up the duct. If your baby has a pus like discharge, they may need an antibiotic and you should see your Optometrist.
I advise parents noticing any of these signs or symptoms to consult your Optometrist as soon as possible. Early detection leads to better treatment outcomes.
Throughout the year children often have eye infections, allergies, and dry eyes. Eye infections can affect one or both eyes and are most common in children. Some eye infections are highly contagious, and you must take care not to infect other people, or even your other eye if only one eye is infected. As a parent, these conditions can be alarming and it is important to know when to come see your Optometrist for evaluation. Medically necessary visits with your Optometrist for these conditions are covered by Alberta Health Care for all age groups including children.
Conjunctivitis – bacterial, allergic or viral – involves inflammation of the transparent membrane that covers the sclera and lines the eyelids.
Bacterial Conjunctiviits or “pink eye” is one of the most common and contagious eye infection particularly among school aged children. When the conjunctiva is infected, the blood vessels become irritated and swell giving the eye a red or pink appearance. Symptoms include: redness, tearing, discharge or pus (matting of the eyes with a green or yellow discharge), itching, burning sensation and light sensitivity. Antibiotics are required to eliminate the bacteria and can take up to two weeks to heal depending on the severity of the infection.
Viral Conjunctivitis is highly contagious as airborne viruses can be spread through sneezing and coughing. This condition can be seen with common viral upper respiratory infections such as the flu or the common cold causing a runny nose, cough, and/or an enlarged lymph gland in front of the ear. Symptoms include: a watery discharge, redness, blurred vision, pain, irritation and light sensitivity. The infection starts in one eye and quickly spreads to the other eye. Unlike a bacterial infection, antibiotics are not effective in treating viruses but rather the use of supportive therapies such as eye drops can help symptoms. The condition is self-limited and will go away on its own.
Allergic conjunctivitis is the result of your child’s immune system reacting to a foreign substance such as pollen, pet dander, dust, or various chemicals. Your child’s body releases histamine as part of an inflammatory response to the foreign substance causing the blood vessels in your child’s eyes to swell and become red and watery. The eyes are typically itchy with a stringy white discharge. Treatment can include having your child avoid the allergen, use of cold compresses, and/or take an antihistamine eye drop especially during allergy season. It is important to note allergic conjunctivitis can be seasonal or perennial (year-round).
Dry eyes is the result of either an insufficient quantity or quality of tears to properly lubricate and nourish your child’s eyes. Dry eyes is chronic, progressive and commonly seen in all age groups in Calgary. Risk factors include medications, contact lens use, computer use, environment, and climate. Symptoms include: blurred vision, burning sensation, dryness, grittiness, itching, sensitivity to light, redness, stinging, tired eyes, eye rubbing, soreness, and tearing. Treatment options are customizable to each child and can include the use of lubricating drops, vitamins, increasing water intake, increasing the number of breaks on the computer, using a humidifier and more.
Blepharitis is an inflammation of the eyelids resulting in redness, crusting and scaling. The eyelids may be itchy or irritated. Blepharitis is commonly seen in conjunction with dry eyes. Treatment includes daily cleansing of your child’s eyelids with lid wipes. In certain cases, an antibiotic cream may be needed. If left untreated, blepharitis can lead to the formation of a stye or chalazion.
Stye or hordeolum is caused by a bacterial infection and produces a tender, red, swollen bump on or within your child’s eyelid that is painful. A Chalazion is nodule or swollen area caused by an oil gland in the eyelid that becomes blocked. The nodule is not red and nor is it tender to touch. Both require warm compresses and sometimes topical antibiotics. In some cases, excision may be required.
Corneal Abrasion occurs after having a foreign body in the eye or scratching the eye. Symptoms include redness, pain, tearing, and sensitivity to light within your child’s eye. An abrasion can be detected by your Optometrist using fluorescein dye drops in the eye and looking at it with a special blue light. Treatment includes an antibiotic until healed.
Dacryostenosis is a blocked tear duct and is very common in newborns and infants. In most cases, the ducts open up on their own by one year of age. Signs include matting of the eye and persistent tearing in one or both eyes of your child. Parents are encouraged to wipe away (using separate cloths for each eye) any discharge with a warm cloth. Gentle massage to ducts is advised to help open up the duct. If your baby has a pus like discharge, they may need an antibiotic and you should see your Optometrist.
I advise parents noticing any of these signs or symptoms to consult your Optometrist as soon as possible. Early detection leads to better treatment outcomes.
Medically reviewed by
Dr. Rabeya Afroz Shomi
MBBS, FCPS, Dhaka Medical
3 Years of Experience
- Written by the Priyojon Editorial Team
